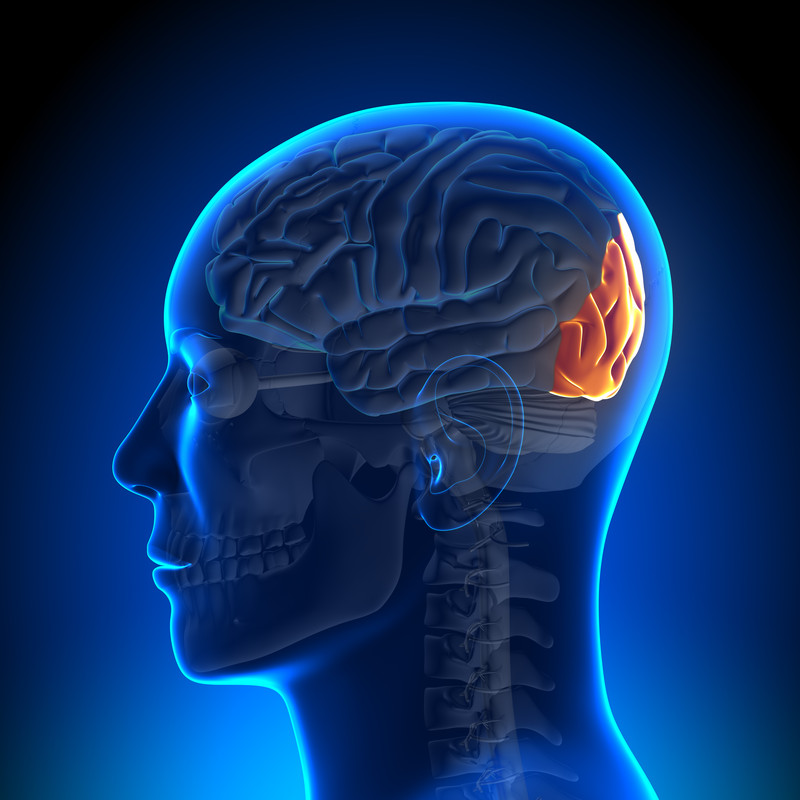
For those who have loved ones with chronic pain, they may know all too well that the condition can take a toll on the person’s cognitive function. Living with chronic pain has been known to increase one’s risk of becoming depressed, irritable, withdrawn, and it can also lead to mood disorders. It can also make people have a more difficult time concentrating and keep them from living a higher quality life.
In the July 2016 issue of The Clinical Journal of Pain, researchers share the details of a study they conducted to highlight the potential to enhance functions, as well as to identify where there are gaps in the literature. This information is helpful to those who work in the field and are trying to help those who may be experiencing cognitive problems as a result of chronic pain (1).
According to the study, cognitive function is commonly disrupted in those who live with chronic pain. However, they also report that it is often an area that is overlooked in pain management settings. This can be problematic, because those seeking assistance for chronic pain may not have the cognitive functioning issue evaluated or addressed, yet they may benefit from it being identified as an issue.
While optimizing cognitive function should be tailored to meet the needs of the individual patient, there are a variety of options to help optimize it. Some of these include getting routine physical activity, having social connections, getting proper sleep, reducing stress, and engaging in mindful meditation. Additionally, some issues that are related to secondary factors, such as mood disorders and sleep problems, may need additional assistance, with some people needing medication to help with the quality of life improvement.
It’s a bit of a catch-22 in that chronic pain can lead to cognitive disruption and have an impact on one’s mood and quality of life. Yet at the same time, research has shown that a patient’s beliefs are important barriers to effective pain management. What people believe about their pain management often ends up influencing how effective it is and what they get out of it. One is essentially affecting the other, and vice versa. Because of this, it’s important that those who have loved ones with chronic pain let their doctors know if there have been changes in the person’s cognitive functioning, and those providing pain management should screen for cognitive function disruption.
While many pain management providers may not be evaluating patients for cognitive function, it does play a big role in someone finding relief and having a better quality of life. Identifying the cognitive function disruptions is the first line in helping to give people what they need to improve their quality of life.
Source:
1. The Clinical Journal of Pain. Optimising Cognitive Function in Persons with Chronic Pain. http://www.ncbi.nlm.nih.gov/pubmed/27479644